Have you ever worked, lived or visited someone in a nursing home or facility and noticed some days they are short handed more than others? Throughout my life I have worked, had family live in nursing homes and visited them so I have seen this in reality for myself. Whether the short staff being CNA’s LPN’s or RN’s there are guidelines and protocol ratios that need to be followed.
According to Cga.ct.gov, Pennsylvania uses a combination of direct care hours with specific staff to patient ratios added. The minimum direct care hours per patient in a facility is 2.7 hours a day, while the minimum staff to patient a ratio is 1:20 nursing staff. However, those are the standard but they also vary on the facilities census & shifts. With 28 PA Code 211.12 in place; a facility with less than 150 residents requires at least one RN at all times. A facility with 251-500 residents require at least 2 RN’s, each shift & those facilities with a large capacity of 1,001 or more requires 8 RN’s on a day shift.
These ratio guidelines are very important and maintained to be held. When the guidelines of nursing staff isn’t met it is easy for mistakes neglect, or issues to occur. One underlying cause of elder abuse and neglect is the problem of understaffing. Understaffing plaques nursing home and facilities extremely, and this isn’t a new issue, it has been happening for decades. Nursinghomeabuseguide.org states that nearly 90% of homes and facilities are currently understaffed.
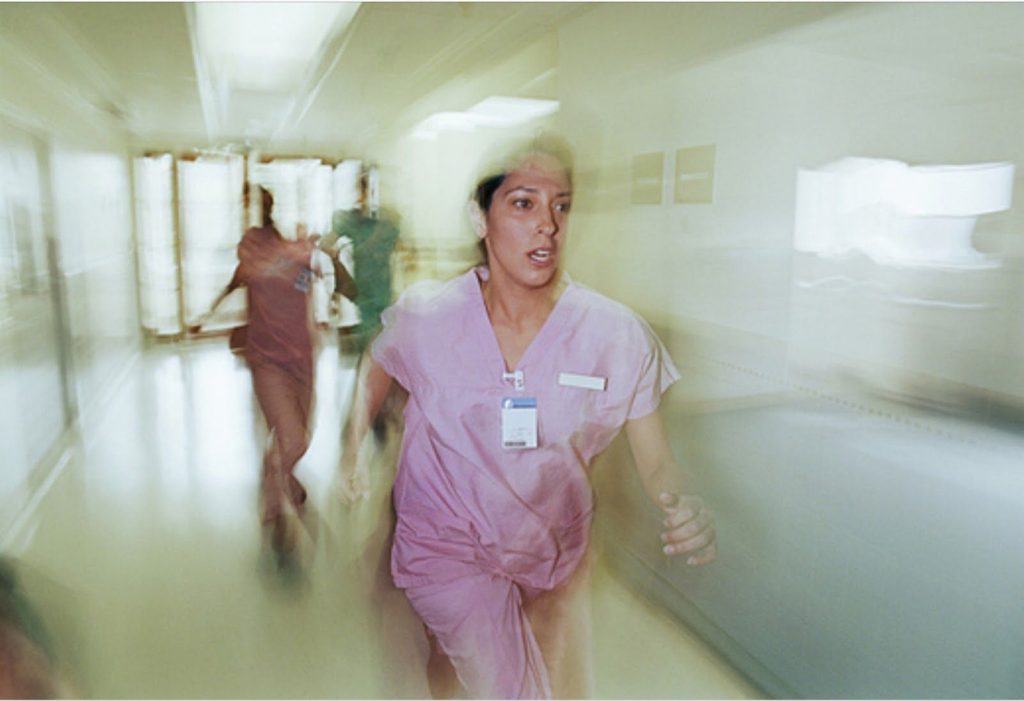
Why are homes and facilities short staffed? There are multiple reasons. One factor is cost, labor costs for a home are high compared to everyday costs, some facilities can not afford to have as much staff as they are required for those reasons. In this case they stretch their existing staff to the point they can’t do anymore. Another factor is the difficult and high stress environment of a nursing home or facility. This makes it hard for the qualified nursing staff to stay athletic job, ultimately leaving the facility, understaffed. When nursing facilities do not obtain enough staff, it doesn’t allow the residents to receive adequate attention they need.
There are a few strategies to cope with understaffing in homes & facilities and these include making sure upper management is aware, aiming for balance & striving for effective communication with in the staff, notice the little successes of a staff member and attribute their success, utilize other staff to their full extent and even looking for an alliance as a model can help. Making the upper management aware of the problem allows there to be the upper hand of hiring temporary help or document the patient to staff volume. Aiming for balance and communication lets staff discuss goals & priorities for the facility. Learning to notice the little successes lets the staff know you care are watching out for their achievements. Most facilities have alternate workers such as agency workers or workers that aren’t licensed the same as the other staff but can do the same job so it’s good to know how to utilize those staff as well as the existing staff. Finally, having an alliance home and facility can be essential, allowing to ask questions, for advice, or possible sharing staff.
If you or anyone else notices constant short staffing in a home/facility, let it be known. Discuss with the management team. By doing this it lets insight from the staff, patient’s loved ones and an outside perspective on the problem.